Managing your symptoms
- I have advanced cancer
- Managing your symptoms
- Fatigue
- Erectile dysfunction (ED)
- Pain
- Hot flashes
- Incontinence
Managing your symptoms
In this section on managing your symptoms, we explore the various manifestations and possible complications related to prostate cancer and its treatments. We provide you with advice and information to help you better understand and cope with these symptoms, as well as strategies to alleviate them and improve your quality of life.
What is it?
Fatigue is the most common symptom reported by people with cancer and it can be acute or chronic. Some of the common symptoms include:
- Sleeping more than usual, or still feeling exhausted after a good night’s sleep
- Tiring quickly during activities, or having lower energy all of the time
- Changes in your emotions (like irritability or mood swings), or a general loss of interest in life
- Trouble concentrating, thinking, or remembering
While feeling tired may seem like a minor inconvenience compared to some of the other issues you experience, it can have a serious impact on your day-to-day activities and quality of life.
Fatigue facts
Studies of prostate cancer patients have found that:
- As many as 74% of prostate cancer patients experienced cancer-related fatigue
- Fatigue is associated with all treatments for prostate cancer
What causes it?
There are many factors that can contribute to fatigue when someone is going through cancer treatment. Some of the common reasons include:
Cancer and cancer treatment
Cancer itself can cause changes in your body, like increasing its need for energy. Chemotherapy and radiation therapy may also cause fatigue as your body works to repair your damaged non-cancerous cells. Treatments that cause side effects like anemia and pain, or that affect your hormones, can also contribute to fatigue.
Poor nutrition
When you have cancer, your body’s need for nutrients and its ability to process those nutrients may change. However, side effects like low appetite, nausea and vomiting can make it difficult to meet your nutrient needs.
Lack of exercise
If you’re normally an active person, the effects of fatigue can feel more pronounced because you don’t have the energy to maintain your usual level of physical activity.
Tips for managing it
Get enough sleep
Keep a regular routine to help you get a good night’s sleep. Do things that relax you leading up to bed time, and make sure your bed, pillows and sheets are comfortable. Avoid sleeping too much during the day as this can make you feel more tired.
Save your energy
Note when your energy is high, and plan activities and appointments around those times of day. You may need to be active for shorter periods, and don’t forget to plan rests as well.
Ask for help
Your family and friends are there to support you, so don’t be shy about taking them up on offers to help. Cooking, chores, driving and helping with pets are just some of the simple ways they can help.
Exercise
Regular exercise (both aerobic and weight training) can help improve your energy levels and reduce fatigue – even something as simple as walking. Be sure to check with your doctor before starting or changing your exercise program.
Eat right
Eat a well-balanced diet and drink plenty of fluids, especially when your energy and appetite are good. In between, try to snack every 2-3 hours.
Manage your mood
Depression and anxiety can increase your feelings of fatigue. Consult our Side effect section on how to look after your emotional well-being.
Work with your healthcare team
If your fatigue has a specific cause, your healthcare team can take steps to treat it, such as nutritional supplements, medicines or blood transfusions, so always keep them up to date on how you’re feeling.
What is it?
Erectile dysfunction (ED) is the inability to get and keep an erection firm enough to have sexual intercourse – even though you can still experience pleasure and have an orgasm. ED is a common side effect of prostate cancer treatments, including surgery (radical prostatectomy), radiation therapy and hormone therapy. Depending on your type of treatment and your age, your ED may be permanent or temporary.
Tips for managing it
If you have ED as the result of prostate cancer treatment, it can be yet another source of frustration in your life. But there are a few ways you can help gain control over your situation:
Don’t give up
Don’t assume you have a permanent problem and nothing can be done. Depending on your treatment you may recover your erectile function, but it can take a long time. In the meantime, try to control your anxiety around sexual encounters and activity, which can make ED worse.
Involve your partner
Honest and open communication can help make sure they know that this isn’t a sign of diminished interest in them, and can help you explore other ways to satisfy one another. Treatment is often more successful when a man involves his partner.
Manage your mood
Stress, anxiety and depression can seriously impact intimacy and erectile function. Be open with your healthcare team about all the issues surrounding your treatment and recovery.
Work with your healthcare team
Depending on the cause of your ED your healthcare team has several options to help you achieve erections, including:
- Medications (including pills, injections, and medicated urethral systems)
- Vacuum constriction devices
- Penile prosthesis
What is it?
People with advanced cancer may experience pain. It can impact you both physically and emotionally, affecting healing and contributing to fatigue, loss of appetite and difficulty sleeping. Depending on your cancer and the type of treatments your received, you may experience pain that is acute (short-term), chronic (long-term) or breakthrough (pain that occurs despite a regular dose of pain medicine).
Tips for managing it
The most important thing to know about cancer pain is that you don’t have to accept living with it. Your healthcare team has many ways to help you manage pain, and there are a few things you can do to help them:
Speak up
Nobody is expecting you to “just deal with it” and nobody will think you’re weak for admitting you’re in pain. The more your healthcare team knows, the better equipped they are to help get your pain under control.
Track your pain
Note when pain happens, what triggered it, where it is, how strong it is (try a simple scale from 1 to 10) and what you did to try and make it better. This kind of information is very helpful to your healthcare team as they try to get your pain under control.
Stick with it
It may take hours or days to get your pain under control. In the meantime, many strong pain medications can have side effects like confusion, lethargy and sleepiness. Don’t let these stop you from sticking with your pain medication regimen! After the first few doses, these side effects usually resolve and you’ll feel more like yourself again.
Work with your healthcare team
You and your healthcare team can put together a pain management plan. This may include:
- Over the counter medication
- Prescription medication
- Treatments that remove the source of the pain e.g. radiation treatments
What is it?
About 50-80% of men on hormonal therapies for prostate cancer will experience some sort of hot flashes. They usually start as a sudden feeling of warmth in the face and chest that then spreads to the rest of the body in waves, lasting anywhere from 2 to 30 minutes. You may also experience sweating, reddening of your skin, a racing heart or feelings of anxiousness. The exact cause of hot flashes is unknown, but it may be related to how hormones interact with a part of your brain called the hypothalamus, which controls body temperature.
Tips for managing them
Hot flashes usually get better as your body gets used to treatment or if medication is stopped, but there are a number of things you can do on a daily basis to help manage them:
- Dress in layers so that you can remove them when you get hot, and wear looser clothing in lighter fabrics (e.g. clothes made with cotton).
- Stick to air conditioned or cool areas with lots of air circulation (e.g. from a fan or open window).
- Avoid hot drinks, caffeine, spicy foods, tobacco and alcohol.
- Practice taking slow, deep breaths when you feel a hot flash coming on, or try relaxing activities like yoga or meditation.
What is it?
Many men who have radiation, TURP (transurethral resection of the prostate) or radical prostatectomy will experience incontinence – the involuntary leakage of urine. The good news is that it’s usually only temporary, and by 6 months after surgery most men will only lose a few drops of urine when lifting, sneezing or coughing (also called stress incontinence). Some men may also experience urge incontinence (also called overactive bladder) – a strong, sudden urge to urinate.
Tips for managing it
Incontinence can make you feel self-conscious and embarrassed, leading to a decreased enjoyment of life. If you’re older, it can also increase your risk of falling as you rush to the toilet. But there are many lifestyle changes you can make to minimize its impact on you as you heal:
- Drink less, especially before bed. Try to avoid alcohol, caffeine, carbonated and sweet drinks, and spicy and acidic foods.
- Schedule regular trips to the bathroom every few hours, and train your bladder by gradually increasing the time.
- Work out your pelvic floor muscles (which help hold in urine) with Kegel exercises. Your doctor can give you advice on how to get started.
Work with your healthcare team
In addition to lifestyle modifications, there are a few ways your healthcare team can further help you get incontinence under control:
- Medications that reduce bladder irritability, decrease bladder spasms or improve bladder emptying
- Surgical procedures to eliminate blockages in the urethra
- Implants to help close off the flow of urine
By looking after your own mental, emotional and physical well-being, you’ll be better equipped to deal with the changes that come from living with advanced cancer and its treatment. The role you play in looking after yourself is just as important as any medicine or treatment.
Other pages that might interest you
Additional Information - I have advanced cancer
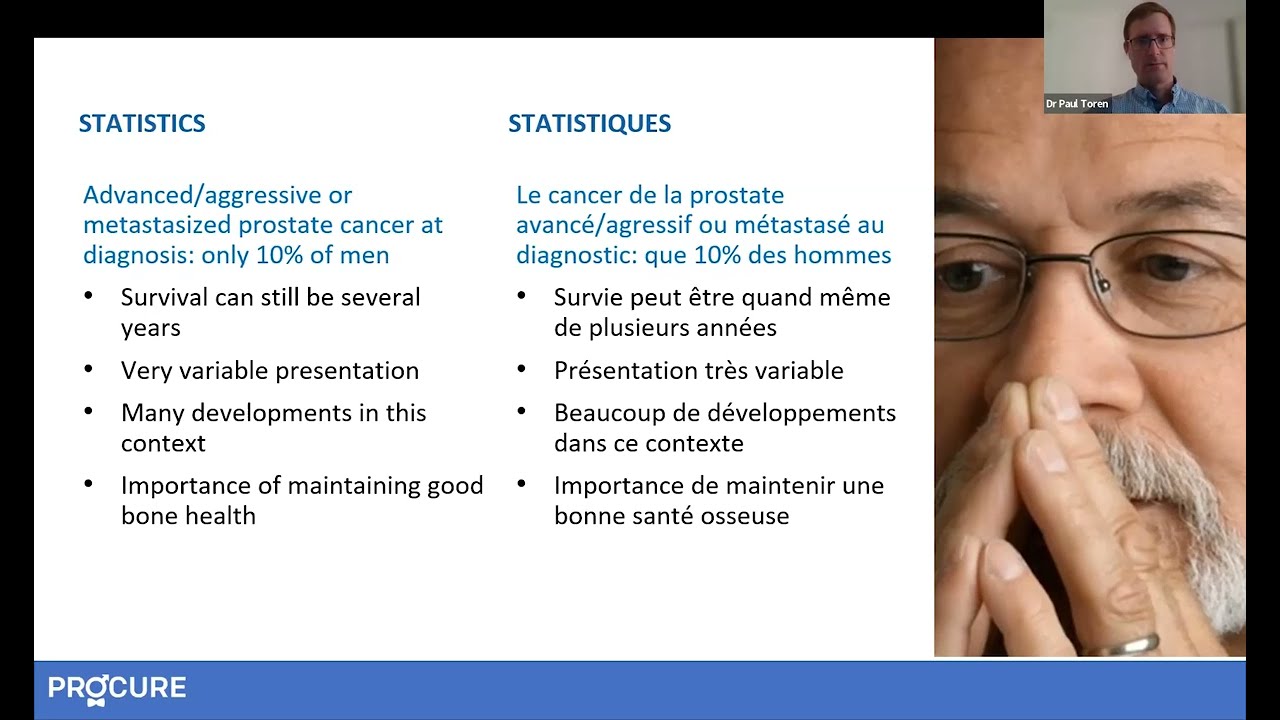
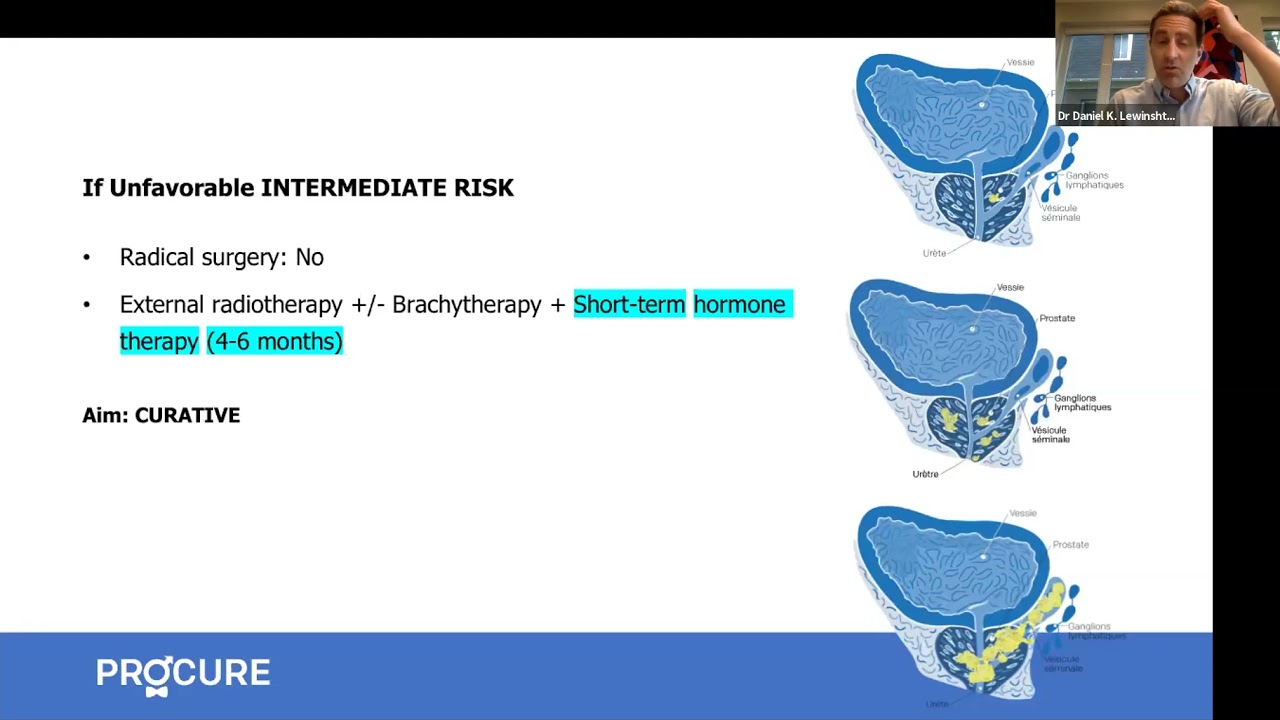
Advanced prostate cancer treatments strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Prostate Cancer Study Results Summaries (2023 ASCO-GU)
Summary of clinical trial results on promising prostate cancer research.
Advanced Prostate Cancer Triple Therapy Study Results (2023 ASCO-GU)
Clinical trial results on triple therapy for advanced hormone-sensitive prostate cancer.
Expert Opinion: Prostate Cancer and Hormone Therapy
What you need to know about hormone therapy and how to manage the side effects of this treatment.
Prostate cancer and nuclear medicine
What about nuclear medicine? Is it suitable for your situation?
Nuclear imaging technologies
Has your doctor suggested prostate imaging tests? Explore options like PSMA PET scans.
Targeted therapy and inherited mutations
If you have a specific genetic mutation, you could benefit from new targeted treatments.
States of prostate cancer following treatment
Do your recent tests show an increase in PSA levels? It could indicate a recurrence.
The role of hormone therapy
Has your doctor recommended hormone therapy? This video is for you!
Advanced prostate cancer treatment strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Advanced prostate cancer treatment
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
When prostate cancer comes back
A recurrence is when the cancer returns after treatment. The main question is, “What’s next?”
How to treat advanced prostate cancer
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
All about hormone therapy
Hormone therapy can reduce tumor size, control cancer, and prolong life. Is it the right treatment for your cancer?
Q-A – New therapies for advance prostate cancer
In this interview, we answer patients’ questions about new therapies for advanced prostate cancer.

Advanced cancer: Factors influencing life expectancy
Being diagnosed with advanced prostate cancer can be overwhelming and frightening. It’s natural to have many questions about your prognosis and what the future holds. One of the key concerns for many patients is understanding their life expectancy. In this article, we’ll explore the factors that can impact life expectancy in advanced prostate cancer and […]

Orchiectomy? Never heard of that word!
Orchiectomy, a form of hormone therapy, involves surgically removing the testicles, depriving the cancer of testosterone.

Food tastes funny…!
I feel like one of the worst effects was losing my taste buds. Everything I tried to eat tasted funny. So why food tastes funny?

Advanced prostate cancer-What should I know?
Advanced prostate cancer-What should I know? The term advanced prostate cancer does not describe just one type of disease, but several. It can be locally advanced, recurrent, metastatic, or resistant to castration. These terms are probably unfamiliar to you and can raise many questions. Here are 5 things you should know Your cancer has returned? […]

When hormone therapy significantly increases overall survival…
The arrival of next-generation hormone therapy to treat non-metastatic castration-resistant prostate cancer provides a significant opportunity for men and their families. Non-metastatic castration resistant prostate cancer treatment NUBEQA® (darolutamide) significantly improves overall survival with a favourable safety profile in men with non-metastatic prostate cancer. Source: Bayer Canada Press Release MISSISSAUGA, ON, June 16, 2020 – Data […]

Can you have a good life despite advanced cancer?
Today, many patients now have access to more than one drug that can help them live longer and improve their quality of life, despite living with advanced cancer. I was diagnosed at the age of 65 and I have been living with my prostate cancer for 20 years. And to all the men who have this […]

Welcome life… Serge’s story
Welcome life… The second part of Serge’s testimony “In my previous testimony, Alone against my diagnosis, I mentioned that when my prostate cancer was announced, a very aggressive cancer, my partner at the time had ended our relationship, the disease – especially cancer – not being her cup of tea. So I found myself in front […]

Alone against my diagnosis… Serge’s story
Alone against my diagnosis… Just like Martin, Serge learns that he has prostate cancer in the prime years of his life, that is to say at the beginning of his fifties (yes age… is relative). What you need to understand is that men who receive a prostate cancer diagnosis are usually much older, well in their sixties […]

You no longer respond to your hormone therapy?
As you know, hormone therapy is mainly used when first treatments fail or when a patient is not a candidate for radical surgery or radiotherapy. On occasion, it can be combined with other treatments, such as radiotherapy. As you also know, hormone therapy may be slowing the growth of prostate cancer, but it cannot cure […]
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.