Radical surgery
Radical surgery
Surgery is a common treatment for prostate cancer. Surgery is used to potentially cure the cancer by completely removing the tumour or to reduce urinary symptoms.
The type of surgery done depends mainly on the stage of the cancer and other factors, such as your age, general health, and life expectancy. Side effects of surgery depend on the type of surgical procedure.

Radical prostatectomy
Radical prostatectomy is the most common surgical procedure for treating localized, low-risk, intermediate-risk or high-risk prostate cancer. It is a major surgery offered to men in good health.
A radical prostatectomy is the total removal of your prostate and the surrounding tissues. It is done as a potential cure for prostate cancer as it removes all cancerous cells. It can be combined with other treatments—for example, surgery followed by radiation therapy if needed.
Pelvic lymph node dissection
Sometimes prostate cancer with only microscopic spread to your lymph nodes can be cured with surgery. How do you know if your cancer has spread to your nodes? Thanks to modern investigative techniques, it is rare that we have to wait until the operation to realize that the cancer is too widespread to be able to perform a prostatectomy.
That being said, if your cancer is more aggressive and you choose to go with radical surgery, your surgeon will remove your major pelvic lymph node groups during the operation. It is not necessary to remove them if your cancer is at a low risk of progression.
Transurethral resection of the prostate
Unlike radical prostatectomies where your prostate and its capsule are removed, a transurethral resection of your prostate (TURP) consists of removing the internal lining of your prostate through your urethra while leaving your prostate capsule in place. This is the most common surgical procedure for benign prostatic hyperplasia (BPH or enlarged prostate).
In general, transurethral resection of the prostate (TURP) is usually given to relieve urinary problems caused by a prostate that has increased in size and is compressing the urethra. It is also used as a palliative treatment to relieve urinary obstructions in patients with advanced prostate cancer who are not healthy enough to undergo radical surgery.
Is it for you
You may opt for this surgery:
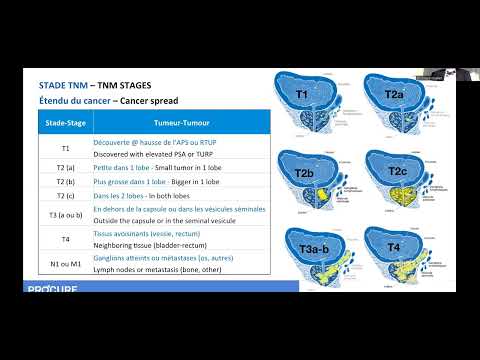
- if you have early stage cancer that has not spread outside the prostate (stage 1 or 2)
- if your cancer has spread locally outside the prostate (stage 3)
- if you have a life expectancy of at least 10 years
- if you are less than 75 years of age, will depend on the individual
- if you are healthy enough to undergo anesthesia and surgery
Reasons for choosing surgery
A radical prostatectomy is effective in the early stages of cancer when it is still confined to your prostate. Chances for recovery are excellent and it offers a high probability for long-term survival (more than ten years).
However, it is also the most aggressive of treatments and therefore has the greatest risk of side effects. Radical prostatectomy is a major surgery. The younger and healthier you are, the more successful your recovery is likely to be. When thinking about surgery, you must consider the effect it will have on your life and weigh the possible benefits against the possible risks.
Surgical techniques
Techniques to surgically remove the prostate include open surgery, hand-assisted laparoscopic surgery and robot-assisted laparoscopic surgery. To learn more about each of these techniques, click here

Advantages of radical surgery
- Completely removes your cancer if there has been no spread outside your prostate
- Provides precise knowledge of the nature and extent of your tumor post-surgery
- Easily assesses the success of surgery with your PSA level six to eight weeks after the operation
- Allows for recourse to radiotherapy or hormone therapy if your PSA level rises
Disadvantages of radical surgery
- There are risks of complications with surgery, as with any major operation
- You will need to stay in the hospital for 1 to 4 days or longer if there are complications
- Different types of radical prostatectomy require, on average, three to six weeks of recovery at home
- If the cancer has spread outside your prostate, the surgeon may not be able to remove it completely
- You will no longer ejaculate and will be unable to have children after surgery.
Risks and complications of surgery
A radical prostatectomy is a major operation, and like any major surgery, there are risks of short-, medium-, and long-term complications. However, they do not affect all men in the same way. It will depend on the type of surgery, the surgeon’s experience, and your overall health.
Short-term
Complications during the operation are rare, but may include:
- Bleeding that may require a blood transfusion
- Injury to the ureter requiring repair
- Trauma or injury to the rectum due to its proximity to the prostate and tumor: it is usually repaired immediately without consequences
- Blood clots in the leg that could travel to the lung
Postoperative
Postoperative complications, upon returning home, may include:
- Pain
- Nausea and vomiting
- Wound infection
- Urinary infection requiring antibiotic treatment
- Constipation due to pain medication
- Bladder spasm due to irritation from the catheter on the bladder walls
- Urinary incontinence and immediate erectile dysfunction in practically all men. These complications are temporary, and things gradually return to normal within the following year for many of them.
Medium to long term
The most common problems associated with radical prostatectomy are:
- Urinary incontinence
- Erectile dysfunction
- Narrowing of the urethra
- For more information on incontinence or erectile dysfunction, see the section on side effects.
Surgery success
The success of surgery and the risk of side effects will depend on the experience and skill of your surgeon. Your surgeon should be able to tell you how many operations he has performed, the success rate of his surgeries, and the rate of side effects in his patients.
The number of surgeries
Surgeons who are regularly in the operating room, e.g., 3 times a month, or who perform at least 20 radical prostatectomies each year, ideally more than 35 per year, have better results, including lower rates of side effects.
The surgeon’s experience
It should be noted that it is not only the number of patients operated on that matters, but also the surgeon’s experience. In this regard, ask him if he can put you in touch with one of his patients. There are also websites where patients give their opinion on doctors. Be careful, as you may be more confused about your surgeon’s skills, as opinions can vary greatly from one patient to another.
Trust
If your surgeon has taken the time to talk to you, answer your questions, and has instilled confidence in his skills, success rate, failures if applicable, and is regularly in the operating room, chances are you are in very good hands. And it is precisely the surgeon’s hands that will make the difference, regardless of whether the surgery is conventional (open) or robotic.

Your doctor has offered you radical surgery to treat your prostate cancer? This section describes this treatment and the precautions to be taken to ensure that everything goes as smoothly as possible.
The medical intervention
Your hospital stay
You will be hospitalized either on the day of or the day before your operation and will stay for anywhere from 24 hours to a few days, if there are no complications.
Duration of the surgery
Two to 4 hours. If your surgeon tells you that he or she can perform this procedure in less than two hours, get a second opinion.
The operation
You will be given general anesthesia or spinal anesthesia (or an epidural like those given to women in labour) so you won’t feel a thing. During the operation, the surgeon will remove your:
- prostate
- seminal vesicles
- area where the prostate meets the bladder (bladder neck)
- part of the urethra that passes through the prostate
- pelvic lymph nodes
Your urinary catheter
While you are still under anesthesia, a urinary catheter will be inserted through your penis to drain urine from your bladder during your healing process. Your catheter will remain in place for 1–2 weeks after your surgery. As urinary incontinence will begin as soon as the catheter is removed, make sure you have absorbent pads in your possession.
The size and nature of your tumour
In the days following your operation, your prostate, seminal vesicles, and removed tissues will be analyzed by a pathologist. This will allow your surgeon to identify the exact size and nature of your tumour.
Your PSA level
Your PSA level should drop to an undetectable level (0) once your prostate has been removed.
Preparation before surgery
Good preparation can make the recovery period after surgery less difficult than expected. Your preparation will play a crucial role in a quicker and less stressful recovery. Before your surgical procedure, you will be asked to come to the hospital for a preoperative visit. Additionally, you will need to sign a release of liability form for your surgeon and the hospital for the risks involved in surgery. This release is mandatory for all surgeries. By reading the following on this page, you will know what to expect and how to cope with it.
Your preoperative visit to the hospital and admission protocol
Before surgery, there are two important steps to follow. The first is your preoperative visit to the hospital, where you will discuss the details of the surgery with the medical team. Then, there is the admission protocol, where you will be prepared for your hospital stay. You will need to sign a release of liability form for your surgeon and the hospital for the risks involved in surgery. This release is mandatory for all surgeries.
The importance of understanding
The side effects related to your surgery
Make sure to have a thorough discussion with your urologist about what the surgery entails, its impact on your quality of life, your sexuality, and the tools available to cope with it. Do not hesitate to reconsider or discuss this option again if you are unsure.
Your prescriptions after your surgery
It will be important to understand the prescriptions you will receive from your urologist and take them when you return home. Your pharmacist can also advise you, but discuss it with your urologist first.
Your Kegel exercises after your surgery
Also, make sure you understand how to resume your Kegel exercises.
Your penile rehabilitation after your surgery
Finally, ask questions about your penile rehabilitation. This involves helping – notably through erection medications – the penis to regain erectile function. Note that this approach is not universally accepted due to the lack of studies on the subject. However, you can still discuss it with your doctor.
- It usually starts soon after your surgery, at a low dose and taken on a weekly basis (frequency may vary from one urologist to another) for several months if you tolerate it.
- Some urologists prescribe these medications (tadalafil, sildenafil, or vardenafil) right away, which you will find in your information envelope or pouch when you leave the hospital.
- Others prefer to wait for the post-surgery follow-up appointment to discuss it.
If your urologist does not address the topic with you during your preoperative visit or follow-up appointment, do not hesitate to bring it up.
A few days before
The hospital Admission service phone call
The day before your surgery, the Admission service will call you to let you know when to come to the hospital. You must arrive 2-3 hours before the scheduled time of your surgery. The surgery time is not definitive. Surgery may take place before or after the scheduled time.
Cancellation
If you are unwell, call your surgeon’s office as soon as possible. If you cannot reach the surgeon, call your hospital’s Admission service.
If your surgery is delayed or canceled due to an emergency, your surgeon will reschedule your surgery as soon as possible.
Prepup
The evening before surgery:
- Take a shower or bath
- Wash your body, starting from the neck down, including your belly button
- Use regular shampoo and soap for your face and hair
- Wear clean clothes to sleep
On the morning of surgery:
- Take a shower or bath
- Put on clean clothes
- Do not apply lotion, wear jewelry, or piercings
- Do not shave the area where you will be operated on
Items to bring to the hospital
- Your health insurance card and hospital card
- Any information related to your private insurance (if you have any)
- Your medications in their original containers
- 1 pack of your favorite chewing gum
- A bathrobe, slippers, loose and comfortable clothes
- Absorbent pads or Depends or Tena incontinence underwear
- Your toiletry kit: toothbrush, toothpaste, mouthwash, comb, deodorant, soap, shaving items, tissues, and earplugs if needed
- Your glasses, contact lenses, hearing aid, dentures with appropriate containers for storage and labeled with your name
- Your cane, crutches, walker labeled with your name
- If you’re tech-savvy, bring your headphones and your music
Note
Please leave all valuables, credit cards, and jewelry at home. The hospital is not responsible for lost or stolen items. Some hospitals will provide a locker for your belongings, but you will be responsible for bringing your lock. Inquire about amenities offered for your personal belongings.
Know that…
You won’t have time to read, as you will be prompted to move, eat, drink, move again, manage your pain, and adjust to this bodily shock. And ideally, if all goes well, you will be discharged from the hospital 1 to 4 days after your surgery.
Questions to my doctor
We invite you to consult our page Questions to ask to your doctor and your healthcare team regarding tests and diagnostic exams for prostate cancer. Asking questions will open up communication, provide information tailored to your situation, and reduce the stress associated with understanding the diagnosis of prostate cancer.

The day of the operation
Make sure you get to the Surgery Pre-Admission office on time
- The admitting attendant will have you sign an admissions form and will ask about your room preference. It is not always possible to get a private or semi-private room.
- The nurse will ask you to put on your hospital gown and will fill in a preoperative checklist with you. You should have been fasting since midnight so your intestines should be empty.
- In some hospitals, you may be asked to wear tight elastic socks to help with blood circulation and prevent blood clots. If this is the case, you should wear them until the nurse tells you to remove them.
The operating room
- An attendant will bring you to the operating room. You will meet your anesthesiologist, the doctor who puts you to sleep, and other members of your surgical team.
- At this stage, there is no point in stressing yourself out or being anxious. You have made the right choice and you are now ready for the next step. Your attitude is vital and will dictate the length of your recovery and facilitate your healing process.
- You will be asleep and feel no pain during surgery.
The waiting room
Your family and friends can wait for you in the room or in the cafeteria. ATMs are usually available in most hospital centres.
During the operation
Your IV
You will be given fluids intravenously until you are able to drink and eat normally. N.B.: When you walk, you will need to push the IV pole with the hand that is not connected to the IV.
Your Jackson-Pratt tube or other post-operative drain
A drain, such as a Jackson-Pratt tube, will be installed in you. The drain is a special tube that prevents blood and fluid from building up inside your abdomen. It consists of two major parts: a flexible tube and a collection bulb. Most patients do not return home with their drain but it is possible. If this is the case, you will be instructed on how to take care of it once you get home.
Your urinary catheter
You will come back from the operating room with a catheter, a tube inserted into your penis called a urinary catheter, which will drain urine from your bladder to a collection bag. You will leave the hospital with your catheter. It is possible for your urine to be tinged with blood—don’t worry.
Your oxygen dose
You might have small tubes in your nostrils to give you oxygen. You will have a small clip on your finger to measure your blood oxygen levels. This is called pulse oximetry. The nurse will adjust the amount of oxygen given to you based on the results and will stop giving you oxygen when you no longer need it.
In the recovery room
After your surgery, you will wake up in the post-anesthesia care unit, also known as the recovery room. This is a quiet place where patients are carefully monitored. You will stay in recovery for several hours.
You will have:
- an oxygen mask, if needed
- an IV line providing liquid
- a urinary catheter (tube) that drains urine from your bladder
- a Jackson-Pratt tube that collects liquid or blood in your abdomen
A nurse will:
- frequently check your pulse and blood pressure
- check your dressings
- make sure that everything is okay
When you are ready, you will be taken to your room. Visitors are not allowed in the recovery room, unless you stay overnight. Your family will be able to visit you when you are in your room.
Pain control
It is normal to feel pain after your surgery. It will feel like a burning or tightening sensation in the area around your incisions. The pain is stronger in the first 24–48 hours and will then gradually decrease.
It is important to control your pain because it will help you to:
- take deep breaths
- move more easily
- eat better
- sleep well
- recover more quickly
- do the things that are important to you
Your nurse may ask you to rate the level of your pain on a scale from 0 to 10. Level 0 means you feel no pain and 10 is the worst pain you can imagine. The staff will want to keep your pain under 4 out of 10. If you are in pain, you need to tell them.The most common possible side effects of pain medication are:
- Nausea and vomiting
- Drowsiness
- Itching
- Occasional headaches
If you experience any of these symptoms, tell your nurse and they will help you. Remember, it is very important that you not wait until the pain is intense to ask for sedatives. If you do, the medication will be less effective and will delay pain relief.
Your mobilization, your exercises, and the objectives to achieve
To prevent pneumonia, blood clots, and muscle mass loss, it will be essential to stay active both in and out of your bed. Click here to discover the expectations of your healthcare team, from when you wake up until your discharge from the hospital, to ensure a safe recovery.
Recovery
The timeline for recovery after radical prostate surgery varies from person to person depending on how their body naturally heals and the severity of the disease before surgery. Access tips to help you in your recovery by clicking here.
Your urinary catheter and bags
You will have 2 drainage bags and a catheter stabilizer. The catheter stabilizer holds the urinary tube in place and keeps it securely attached to your leg. The small bag is for daytime and the larger one is for nighttime. Refer to the care sheet for your urinary catheter here.
Maintenance of your Jackson-Pratt drain
The Jackson-Pratt drain is connected to a container that resembles a grenade called a bulb. This container holds fluid draining from the incision, aiding in healing. Refer to the care sheet for your drain here.
Activities
Resuming activities at home
- Continue walking several times a day. Gradually increase the distance until you reach your usual activity level. Most patients do not have many restrictions.
- Do not drive while taking painkillers
- Avoid lifting weights of 5-10 pounds (2-4 kg) for at least 4 weeks to reduce the risk of hernia.
- Your surgeon will decide when you can return to work. This will depend on your recovery and the type of work you do.
- You will likely return to work a few weeks after your surgery provided you don’t have to lift heavy objects.
- Wait 6 weeks before engaging in sports requiring sudden movements (e.g., tennis, badminton, jogging, downhill skiing) and gradually ease into them.
- If you are an avid cyclist and your surgery goes well, there are no postoperative complications, and you recover continence well, you could saddle up 8 to 12 weeks after the operation. However, it’s best to get clearance from your doctor.
Ask your family and friends for help
- For transportation
- For meal preparation
- For laundry
- For grocery shopping
- For housekeeping
For swimming
Not before at least 4 weeks. You must wait until the staples and approximation stitches, drains, absorption of absorbable stitches, and cessation of wound drainage…
For travel
Local and regional: Upon hospital discharge provided you make frequent stops every hour.
International: Avoid destinations where medical services are not readily available (to be discussed with your doctor).
When to call your doctor
You will need to monitor certain signs and symptoms upon returning home to know when to contact your doctor or when to go to the emergency room. Click here to learn more (see content transferred to a new invisible page entitled When to call your doctor).
Medical follow-up
Medical certificate
If you need a medical certificate, remember to request it directly from your surgeon, at least the day before your hospital discharge.
Medical follow-up
You should see your urologist within 4-6 weeks after leaving the hospital. Then, you will have regular follow-up appointments (every 3 to 6 months). After five years without recurrence, if all goes well, follow-up becomes annual.
Success rate
It is impossible to establish a general success rate with surgery.
- This varies depending on each case because it is necessary to consider the diagnosed grade of the tumor, its stage of spread, and the PSA level before treatment.
- The lower these data are, the better the chances that the patient will be definitively out of the woods.
PSA test
Your urologist will perform a PSA test each time as it is the best predictor of prostate cancer recurrence. He sometimes also performs a rectal exam.
Your PSA level
After the operation, the PSA level should be undetectable (0) since there is no longer a prostate to produce the antigen. At each follow-up appointment, your urologist will assess three parameters:
- if the PSA level increases
- how long after the operation this occurred
- and how long it takes for this level to double (its velocity)
Recurrence
If the PSA level starts to rise, the doctor will monitor how long it takes to double. The shorter these periods are, the greater the risk of recurrence, and the more aggressive the recurrence will be. For example, a PSA level that starts to rise eight months after surgery and doubles in six months is much more concerning than a PSA level that starts to climb three years after surgery and takes a year to double. Typically, your urologist will be concerned if your level reaches 0.1 and may decide to administer salvage treatment. A PSA level of 0.2 indicates that you are officially in recurrence.
If necessary, radiotherapy and/or hormone therapy may be prescribed.
Remission
You will be followed for at least five years after your surgery. After five years without recurrence, if all goes well, the risk of the cancer returning is low.
Side Effects
The most common issues associated with radical prostatectomy are urinary incontinence and erectile dysfunction.
Urinary Incontinence
Following surgery, nearly all men experience a transitional period of urinary incontinence. Its duration varies from person to person depending on the severity of the disease, age, and overall health. It generally improves over time and with the practice of specific exercises such as Kegels. Numerous strategies can help you manage urinary difficulties after prostate cancer treatment. To learn more about urinary incontinence, refer to our page on urinary disorders.
Erectile Dysfunction
A certain percentage of men regain erectile function within 6 to 36 months after surgery. The speed at which sexual function improves depends on preoperative sexual function, age, overall health, and preservation of erectile nerves during surgery. In most cases, erectile problems can be effectively treated. In the meantime, if you need assistance in navigating this challenging period, don’t hesitate to speak with a sex therapist, physicians, nurses, or our healthcare professionals. To learn more about erectile dysfunction, refer to our page on sexual disorders.
Additional Information - Treatment options
Medical monitoring and care management
Are you undergoing treatment for prostate cancer? Various approaches can help monitor it.
Everything to know about radical surgery
Considering radical surgery for your cancer treatment? Watch this webinar to learn about the procedure, its benefits, drawbacks, and suitability for you.
Urinary and sexual problems after treatment
Prostate cancer treatments can lead to side effects, such as erectile dysfunction and urinary incontinence, which vary in intensity and duration.
Surveillance, surgery or radiation therapy?
Diagnosed with prostate cancer? Several treatment options are available based on the stage, age, and your health.
Active surveillance as a treatment option?
Did you know that in many cases it is not necessary to treat prostate cancer?

I was told about leaks, not incontinence
It is not uncommon to have calls from patients asking us why they suffer from incontinence following radical surgery to treat their prostate cancer.

I have 4 treatment options; confused, you say?
If being diagnosed with prostate cancer is a massive blow for men, the treatment options can quickly become a headache…

Active surveillance in 5 points
As surprising as it may seem, your doctor may prefer to wait before starting treatment.

Permanent brachytherapy: What exactly is it?
Permanent brachytherapy often called low dose rate brachytherapy, administers very small doses of radiation. They are emitted from small sources containing radioactive iodine, called “iodine 125”. These sources look like grains of rice. They stay in your prostate forever. However, their radioactivity decreases over time. After 6 months, 95% of the radioactivity has disappeared. The presence of these sources does not cause any long […]

Radical surgery: 5 points to remember
If you’ve been diagnosed with prostate cancer, your doctor will consider many factors before recommending the best treatment. For many of you, this may mean completely removing the prostate, which is radical surgery. Here are 5 points to remember if you are considering this option. Radical surgery: Is it for you? Radical surgery is the most common […]
Conventional or robotic surgery?
Here is a typical case of concern from a patient who has opted for radical surgery as a treatment for his cancer and who asks the famous question: Which surgery is better? Conventional or robotic surgery? Before answering it, let’s take a look at the context in which the question was asked of our nurses […]

Choice between radical surgery or radiotherapy?
Unless you are not a candidate for either option, there are generally no strict rules for deciding whether radical surgery or radiotherapy is preferable as a treatment. If your cancer is really confined to your prostate, it can be cured with surgery or radiation therapy. However, to benefit from a cure, your life expectancy must be […]

Recovery timeline after surgery
Recovery timeline after surgery, that is after radical prostate surgery, varies from person to person depending on how their body heals naturally and the severity of the disease before surgery. Here are some tips to help you with your recovery timeline. Plan your return home After surgery, you will not necessarily have the energy to […]

What is successful active surveillance
Is it possible to achieve successful active surveillance? Of course. Does this mean your cancer will never progress? Not at all. But in 65-70% of cases, cancer does not progress because the patient was a good candidate for this type of treatment option. Having prostate cancer does not necessarily mean that you will be treated. […]
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.